

International symposiumControversies in glaucoma

Primary angle closure glaucoma (PACG) is still one of the leading causes of the irreversible blindness. The risk of bilateral blindness due to PACG is three times higher than in primary open angle glaucoma.
Among many urgent problems associated with primary angle closure disease (PACD), the most important one is to determine the treatment algorithm for primary angle closure suspect (PACs) and primary angle closure (PAC) to avoid the disease progression.
The present review, that is devoted to the problem of PACD, demonstrates how early detection of this condition, determination of its prognosis, and the formation of a personalized treatment algorithm allow preventing the development of one of the most severe forms of ophthalmopathology. Modern visualization technologies of the structures of the anterior and posterior segments, as well as the analysis of the data obtained by means of machine learning methods, make it possible to achieve the most personalized approach of the treatment of primary angle closure that corresponds to the principles of 3P medicine.

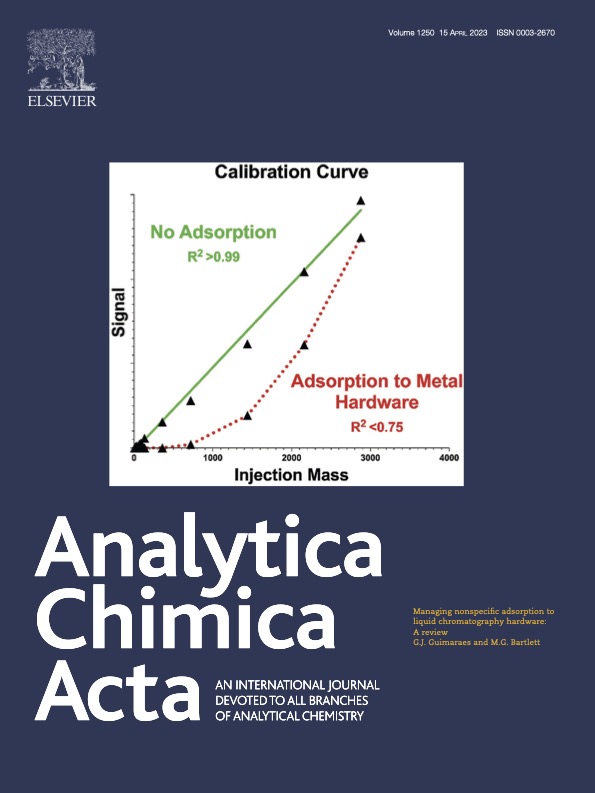
Novelty and similarity are complex concepts that have numerous applications in various fields, including biology and medicine. Novelty detection is a technique used to determine whether a dataset is different from another dataset considered as a standard. Similarity detection is a technique used to determine whether two datasets belong to the same population. Novelty and similarity are closely related concepts; however, they are not complementary. Novelty is a much more popular one, and there are many publications about it. Similarity is, in fact, a new concept that has not yet been explored in depth. Classical statistics offers a large number of tools suitable for detection of similarity, mostly in the univariate case. At the same time, this topic has been insufficiently studied in the field of machine learning. This paper suggests several principles which are important for this research and also present a method for the detection of both novelty and similarity. The method uses a one-class classifier, known as Data- Driven Soft Independent Modeling of Class Analogy (DD-SIMCA). Three examples illustrate our approach. The first one uses simulated data and demonstrates the performance of DD-SIMCA for the detection of novelty. The second example uses a realworld data and studies similarity of two groups of patients who participate in the evaluation of the effectiveness of the treatment of primary angle-closure glaucoma. The third example comes from medical diagnostics. This is a real-world publicly available data used for comparison of various classification algorithms.


PURPOSE. To determine the predictors of hypotensive effectiveness of lens extraction (LE) with intraocular lens implantation in patients with primary angle closure (PAC) using machine learning. METHODS. This prospective study included 30 patients with PAС, aged 41 to 80 years, who underwent LE. The observation period lasted 1 month. All subjects underwent swept source optical coherence tomography (SS-OCT). Thirtyseven parameters were analyzed in total, including spherical equivalent (SE), corrected distance visual acuity (CDVA), intraocular pressure (IOP), Shaffer angle opening degree, lens opacity, choroidal thickness in the macula, axis length (AL), anterior chamber depth (ACD), lens vault (LV), iris curvature (ICurv) and thickness (IT750), anterior chamber angle opening distance (AOD), trabecular-iris space area (TISA). The difference in intraocular pressure (ΔIOP) after the intervention relative to the baseline was used as the criterion for treatment success. Machine learning based on multivariate statistical data analysis was used along with standard methods of descriptive statistics. RESULTS. After treatment, IOP decreased from 25.5±2.3 mm Hg up to 17.2±1.19 mm Hg (p=0.000) while the number of local hypotensive drugs statistically significantly decreased (from 0.63±0.49 to 0.07±0.25, p=0.001). Predictors of ΔIOP were: advanced age (B-coefficient=0.235), male gender (B=-0.243), presence of early cataract (B=0.274), low CDVA (B=-0.06), high values of preoperative IOP (B=0.267), SE (B=0.437), LV (B=0.237) and ICurv (B=0.260 in the nasal and 0.232 in the temporal sectors, respectively), as well as low values of IT750 (B=-0.142 and -0.146 in the same sectors, respectively), ACD (B=-0.367), AL (B=-0.487), anterior chamber angle profile parameters. CONCLUSION. Machine learning was used to determined the following predictors of the hypotensive effect of LE: advanced age, male gender, high initial IOP, spherical equivalent and lens vault, the presence of early cataract, steep and thin iris, shallow anterior chamber, short axis length and narrow anterior chamber angle.


PURPOSE. To develop a personalized approach to sele- cting a treatment method for primary angle closure (PAC) based on a comparison of the predicted hypotensive effect of laser peripheral iridotomy (LPI) and lens extraction (LE). METHODS. This prospective study included 60 patients (60 eyes) with PAC aged 41 to 80 years. LPI was performed on 30 eyes and LE on 30 eyes. All patients underwent swept-source optical coherence tomography (SS-OCT) of the anterior and posterior segments of the eye before and 1 month after treatment. A set of 37 clinical and anatomical parameters of each patient was evaluated. The hypotensive effect of the surgery was considered to be the magnitude of the decrease in intraocular pressure (IOP) after the intervention relative to the baseline. The principal component regression method was used to develop regression models predicting the hypotensive effect of treatment. RESULTS. An innovative step-by-step algorithm for choosing a treatment method for PAC (LE or LPI) has been developed. The first step is to measure and take into account 4 clinical and anatomical parameters of the patient: gender, IOP, axial length of the eye (AL), and anterior chamber depth (ACD). The second step is to calculate the predicted difference in hypotensive effect (Ind_Short) using the formula Ind_Short=B0+B1·Gender+B2·IOP+B3·AL+B4·ACD, where B0=16.8; B1=-0.28; B2=0.24; B3=-0.65; B4=-2.36; male gender is 0 (zero) and female gender is 1. The third step is to compare the obtained result with zero: LPI is the preferred method if Ind_Short is less than 0, otherwise LE. CONCLUSION. The developed step-by-step algorithm in- volving the use of machine learning methods allows a personalized approach to the treatment of primary angle closure.

This article reviews literature on the use of artificial intelligence (AI) for screening, diagnosis, monitoring and treatment of glaucoma. The first part of the review provides information how AI methods improve the effectiveness of glaucoma screening, pres- ents the technologies using deep learning, including neural networks, for the analysis of big data obtained by methods of ocular imaging (fundus imaging, optical coherence tomography of the anterior and posterior eye segments, digital gonioscopy, ultrasound biomicroscopy, etc.), including a multimodal approach. The results found in the reviewed literature are contradictory, indicating that improvement of the AI models requires further research and a standardized approach. The use of neural networks for timely detection of glaucoma based on multimodal imaging will reduce the risk of blindness associated with glaucoma.

The second part of the literature review on the application of artificial intelligence (AI) methods for screening, diagnosing, monitoring, and treating glaucoma provides information on how AI methods enhance the effectiveness of glaucoma monitoring and treat- ment, presents technologies that use machine learning, including neural networks, to predict disease progression and determine the need for anti-glaucoma surgery. The article also discusses the methods of personalized treatment based on projection machine learning methods and outlines the problems and prospects of using AI in solving tasks related to screening, diagnosing, and treating glaucoma.


<b>Précis:</b> Treatment strategy of primary angle closure (PAC) is not clear due to the large number of clinical and anatomic-topographic parameters in PAC, influencing the treatment algorithm. Using the machine learning method DD-SIMCA, we justify the expediency of early lens extraction (LE) in PAC
<br><b>Purpose:</b> To compare the anatomic and functional efficacy of LE and laser peripheral iridotomy (LPI) in patients with PAC using Machine Learning.
<br><b>Materials and Methods:</b> This prospective study included 120 patients aged 41–80 years: 60 eyes with PAC, 30 with PAC suspects, and 30 with healthy eyes (control). Thirty PAC eyes with intraocular pressure (IOP) up to 30 mm Hg were treated using LE with intraocular lens implantation and 30 eyes with LPI. All subjects underwent Swept Source optical coherence tomography. We analyzed 35 parameters of each eye including the lens vault, the choroidal thickness, the anterior chamber angle, and iris specifications such as iris curvature. Considering the correlations between them, the machine learning method DD-SIMCA 1-class classification was applied: the proximity of each sample to the target class (control) was characterized by the total distance to it.
<br><b>Results:</b> After LE, IOP was significantly lower than after LPI (P=0). Every third eye with PAC after LE reached the target class: specificity according to DD-SIMCA equals 0.67. This was not observed for the eyes after LPI: specificity equals 1.0. After LE, all parameters of the anterior chamber angle did not differ from the control (all P>0.05). After LPI, there was an increase in anterior chamber depth (P=0) and a decrease in lens vault (P=0), but results comparable to the control were achieved only for iris curvature (P=1.000).
<br><b>Conclusion:</b> The efficacy of LE in PAC is higher than LPI due to the better postoperative anterior chamber topography and lower IOP. This study lends further clinical and anatomic support to the emerging notion of LE as an effective treatment for PAC.


<b>Patent holder:</b>Kurysheva N.I, № 2023106565; statement. 21.03.2023; Publ. 08.06.2023, Bull. № 16. – 7 с
The invention relates to medicine, namely to ophthalmology, and can be used to determine the tactics of surgical treatment of patients with primary closure of the angle of the anterior chamber of the eye (ACE) with intraocular pressure less than 30 mm Hg. For this purpose, the intraocular pressure, the length of the anterior-posterior axis of the eye, the depth of the anterior chamber of the eye are determined for this category of patients, and gender is taken into account. The Ind value is calculated using the developed mathematical formula. If the Ind value is less than zero, peripheral laser iridotomy is performed. If the Ind value is greater than zero, lensectomy is performed. The invention allows for an adequate choice of the method of surgical treatment of patients with primary closure of the angle of the anterior chamber of the eye with the achievement of the maximum hypotensive effect for the prevention of the development of glaucomatous optic neuropathy with ACE into primary angle-closure glaucoma. 2 pr.


<b>Purpose:</b>To compare the anatomical and functional effectiveness of lensectomy (LE) and laser peripheral iridotomy (LPI) in patients with primary anterior chamber angle closure.
<br><b>Methods:</b>This prospective study included 120 patients aged 41 to 80 years (60 eyes — primary angle closure (PAC), 30 — primary angle closure suspects (PACs), 30 eyes — without ophthalmic pathology). 30 PAC eyes were treated using LE with intraocular lens implantation, and 30 eyes with LPI. All subjects underwent swept source optical coherence tomography (SS-OCT). The following parameters were analyzed: spherical equivalent (SE), uncorrected and corrected distance visual acuity, intraocular pressure (IOP), Shaffer grade of angle opening, lens opacity, goniosynechiae, choroidal thickness in the macular region, axial length (AL) of the eye, anterior chamber depth (ACD), lens vault (LV), iris curvature (ICurv), iris thickness at 750 μm from scleral spur (IT750), angle opening distance (AOD500, AOD750), iridotrabecular space area (TISA500, TISA750). Along with standard descriptive statistics methods, machine learning methods were used, including Data Driven Soft Independent Modelling of Class Analogies (DD-SIMCA).
<br><b>Results:</b>Every third eye with PAC had reached cont- rol group values after LE (DD-SIMCA specificity 0.67), which was not the case after LPI (DD-SIMCA specificity 1.0) with the probability of getting into the control group estimated as 0.01. After LE, all parameters of the anterior chamber angle did not significantly differ from the norm (p>0.05 for all), while ACD, ICurv even exceeded the norm (p=0.000). After LPI, there was a deepening of the ACD (from 2.34±0.28 mm to 2.36±0.280 mm, p=0.000) and a decrease in LV (from 0.864±0.120 μm to 0.843±0.110 μm, p=0.000), however, the result comparable to control was achieved only in ICurv (p=1.000). After LE in PAC, all parameters, including uncorrected visual acuity, SE, ACD, LV, iris profile, Shaffer grade of angle opening, and AOD500, AOD750, TISA500, TISA750 parameters in the superior and inferior sectors had advantages over those in PACs without treatment (p<0.05). After LPI, an improvement in a number of parameters was also achieved compared to LPI: ICurv, Shaffer grade of angle opening, AOD500, AOD750, TISA500, TISA750 in the superior sectors and AOD500 in the inferior sector (p<0.05).
<br><b>Conclusion:</b>The effectiveness of LE in PAC is higher than LPI due to the better postoperative anterior chamber topography and lower IOP. Both treatments, especially LE, improve these parameters compared to PACs. Lens extraction is the treatment of choice at the early stages of primary angle closure.

In this paper we analyze the set of anatomical and clinical parameters which are known to affect the hypotensive efficacy of laser peripheral iridotomy (LPI) and lensectomy (LE) in primary anterior chamber angle closure (PAC). The study included 60 patients with PAC who underwent LE or LPI. The treatment efficacy was evaluated using reduction of intraocular pressure (ΔIOP) as the response. The Partial Least Squares regression was applied using 37 anatomical and clinical parameters obtained before a treatment as the predictors. We observed a significant decrease in IOP in both groups after the treatments, but LE has the greater ΔIOP compared to LPI. Variable selection was applied to determine the predictors which primarily affect the outcome. The study identifies the general and specific factors of the IOP decrease in LPI and LE that may be explained by the mixed mechanisms of PAC development.

<b>Background:</b> Primary angle closure glaucoma (PACG) is still one of the leading causes of irreversible blindness, with a trend towards an increase in the number of patients to 32.04 million by 2040, an increase of 58.4% compared with 2013. Health risk assessment based on multievel diagnostics and machine learning–couched treatment algorithms tailored to individualized profile of patients with primary anterior chamber angle closure are considered essential tools to reverse the trend and protect vulnerable subpopulations against health-to-disease progression.
<br><b>Aim:</b> To develop a methodology for personalized choice of an effective method of primary angle closure (PAC) treatment based on comparing the prognosis of intraocular pressure (IOP) changes due to laser peripheral iridotomy (LPI) or lens extraction (LE).
<br><b>Methods:</b> The multi-parametric data analysis was used to develop models predicting individual outcomes of the primary angle closure (PAC) treatment with LPI and LE. For doing this, we suggested a positive dynamics in the intraocular pressure (IOP) after treatment, as the objective measure of a successful treatment. Thirty-seven anatomical parameters have been considered by applying artificial intelligence to the prospective study on 30 (LE) + 30 (LPI) patients with PAC.
<br><b>Results and data interpretation in the framework of 3P medicine:</b> Based on the anatomical and topographic features of the patients with PAC, mathematical models have been developed that provide a personalized choice of LE or LPI in the treatment. Multi-level diagnostics is the key tool in the overall advanced approach. To this end, for the future application of AI in the area, it is strongly recommended to consider the following: <br>1. Clinically relevant phenotyping applicable to advanced population screening; <br>2. Systemic effects causing suboptimal health conditions considered in order to cost-effectively protect affected individuals against health-to-disease transition; <br>3. Clinically relevant health risk assessment utilizing health/disease-specific molecular patterns detectable in body fluids with high predictive power such as a comprehensive tear fluid analysis.

It is proposed to use DD-SIMCA method, and, particularly, Full Distancse (FD) as an analytical signal that characterizes each sample in the frame of a classification task. The approach is demonstrated using medical data. FD values help to assess the proximity of each patient to the target class of the control (healthy) subjects. Furthermore, the FD values are used as a response in the PLS model, which predicts the distance of the subject (object) to the target class after a certain treatment and, therefore, the probability of recovery for each person. This enables the application of the personalized medicine. The proposed approach can be used not only in medicine, but also in other fields, e.g., restoration work to preserve and restore cultural heritage sites.

The article reviews literature data on the search for predictors of the success of laser peripheral iridotomy (LPI) and lensectomy in the early stages of primary angle closure disease (PACD) and presents a trend analysis of the studies conducted on individuals identified as primary angle closure suspects (PACs) and those with primary angle closure (PAC). The concept of the review was de- termined by the ambiguous choice of treatment for patients at the stage of PAC onset. Determining the success predictors of LPI or lensectomy plays a key role in optimizing the treatment of PACD. The results of literature analysis are contradictory, which indi- cates the need for further research taking into account modern methods of visualization of the eye structures such as optical coher- ence tomography (OCT), Swept Source OCT (SS-OCT), and the use of uniform criteria for evaluating the effectiveness of treatment.


<b>Purpose:</b> (T)o determine the anatomical and topographic features of the anterior and posterior segments of the eye in primary angle closure (PAC) and compare them with those in the primary angle closure suspects (PACs) and in controls.
<br><b>Methods:</b> (T)his prospective study included 120 patients aged 41 to 80 years (60 eyes — PAC, 30 — PACs, 30 eyes — without ophthalmic pathology). The studied parameters included spherical equivalent (SE), intraocular pressure (IOP), choroidal thickness in the fovea (CTf), axial length (AL), anterior chamber depth (ACD), lens volume (LV), iris curvature and its thickness, anterior chamber angle profile: AOD500, AOD750, TISA500, TISA750.
<br><b>Results:</b> The PAC eyes differed from the control eyes by increased SE, LV, IOP, iris curvature, CTf, reduced ACD, AL, and the anterior chamber profile (AOD500, AOD750, TISA500, TISA750) in vertical sectors (p<0.01). Iris thickness was comparable between the groups.<br>The PAC eyes differed from the PACs by increased SE, LV, IOP, reduced ACD, AL, AOD500 in the superior sector, and the profile of the anterior chamber angle in the inferior sector (p<0.01). Iris thickness, its curvature, as well as the profile of the anterior chamber in the upper sector and CTf were comparable.<br>Threshold values that distinguish the PAC eyes and the PACs were determined: LV — 0.656 mm, AOD500 — 0.131 mm, TISA500 — 0.051 mm2, TISA750 — 0.093 mm2 in the lower sector and IOP 21 mm Hg. In the multifactor model adjusted for age, gender and AL, a negative correlation of iris thickness with CTf was established both in the PAC eyes and the PACs (all p<0.01), but not in the controls (all p>0.01).
<br><b>Conclusion:</b> (P)arameters of the PAC eyes and the PACs significantly differ from the norm. LV and the anterior chamber profile in the inferior sector are the most informative for differentiating the PAC eyes from the PACs. Negative correlation between the iris and the choroidal thickness suggests that the choroid plays a role in the pathogenesis of primary angle closure disease.

<b>Purpose:</b> (P)urpose. To evaluate the application of the principal component analysis (PCA) and DD-SIMCA in a comparative analysis of the surgical treatment of primary angle closure.
<br><b>Material and methods:</b> (h)e prospective study included 90 patients. Group 1 — 30 patients with primary angle closure (PAC) with planned laser peripheral iridotomy (LPI). Group 2 — 30 patients with PAC, with planned phacoemulsification with intraocular lens implantation (PE+IOL). Group 3 — 30 eyes without ophthalmic pathology. All subjects underwent SS-OCT. Thirty-seven parameters were analyzed, including intraocular pressure, choroidal thickness in the macula, anterior chamber depth, lens vault, iris curvature and thickness, angle opening distance, and iridotrabecular space at 500 μm and 750 μm from the scleral spur. Since all these parameters correlate with each other, machine learning methods were used: PCA and the DD-SIMCA one-class classification method. For this purpose graphs of scores and loads in the PCA model for groups 1 and 2 were plotted. In the score plot, patients with PAC with average and extreme eye parameters were identified, and in the loading plot, relationships between the parameters of patients with PM were used to analyze correlations in the future. In the DD-SIMCA method, group 1 is taken as representatives of the target class. Results. A classification model based on 2 principal components with a given type I error α = 0.01 demonstrated a sensitivity of 100 % for patients in its own group and a sensitivity of 93 % for patients in group 2. These results confirm similarity of group 1 and group 2. The specificity for the control group was 100 %, and this group located far from the target group.
<br><b>Conclusion:</b> (M)achine learning methods make it possible to compare groups with multivariate and correlated parameters. PCA allows the identification of patients with extreme parameters and the evaluation of correlations between multiple parameters. DD- SIMCA confirms the validity of comparing the results of treatment with LPI and FE + IOL.

To review the literature devoted to the problem of primary anterior chamber angle closure (PAC) and the development of this pathology from glaucoma suspect to primary angle closure glaucoma. The paper includes a trend analysis of the studies concerning primary angle closure suspects (PACS). The concept of this review is conditioned by the conflicting strategies for treating patients with initial PAC without glaucomatous optic neuropathy. Solving the problem of angle closure plays a key role in preventing the development of PAC glaucoma, which is the world’s leading cause of irreversible blindness. This part of the review provides information on the frequency and rate of disease progression in PACS. The analyzed literature data is contradictory and indicates the need for further search that would consider a standardized approach to defining the concept of PAC disease, demographic factors and unified examination methods for generalizing and systematizing data in order to draw out unified treatment recommendations.

To review the literature devoted to the search of predictors of primary angle closure (PAC) progression as an important link in the pathogenesis of primary angle-closure glaucoma. This part presents a cluster analysis, describes the mechanisms of PAC development, and considers the studies aimed at discovering the risk factors for the progression of primary angle closure suspect into true angle closure. The results of the analyzed literature are ambiguous, indicating the need for further research that would involve strict inclusion criteria, and a standard approach to defining the primary angle closure disease and expanding the diagnostic parameters, in which a key role belongs to anterior segment optical coherence tomography (AS-OCT).


<b>Purpose:</b> (T)o demonstrate the advisability of early lens extraction in the treatment of primary angle closure disease in clinical practice.
<br><b>Methods:</b> (T)he study presents three clinical cases with patients at different stages of primary angle closure disease (PACD). The first one is related to the development of a bilateral acute attack of primary angle closure (PAC) that happened in the intensive care unit during treatment for acute respiratory distress syndrome (ARDS) associated with COVID-19 pneumonia in a patient with a previously undiagnosed PACD. The second case demonstrates the progression of glaucomatous optic neuropathy (GON) in early primary angle-closure glaucoma (PACG) after laser peripheral iridotomy (LPI) and delayed selective laser trabeculoplasty (SLT) in a patient with increased lens thickness. The third example illustrates the progression of advanced PACG in the right eye (OD) and moderate PACG in the left eye (OS) due to formation of goniosynechiae after bilateral LPI, which required transscleral diode cyclophotocoagulation (TSCP) in OD and trabeculectomy in OS. Subsequently, bilateral cataract phacoemulsification with intraocular lens implantation (CPE+IOL) and SLT were performed.
<br><b>Results:</b> (I)n the first clinical case, advanced PACG developed in both eyes within 2 months. After bilateral LPI, trabeculectomy, compensation of intraocular pressure (IOP) was achieved, visual functions stabilized.<br>In the second clinical case, 5.5 years after LPI and SLT, an increase in the thickness of the lens was revealed (in OD by 0.2 mm, in OS by 0.48 mm). GON did not progress in OD (thinning rate of the retinal nerve fiber layer was 0.94 μm/year, p=0.32) and the progression rate in OS was -1.04 μm/year (p=0.018). Taking into account the lens-involved mechanism of PACD progression, bilateral CPE+IOL was recommended. In the third clinical example, IOP remained elevated after bilateral LPI, TSCP in OD and trabeculectomy in OS as a result of goniosinechiogenesis, and therefore CPE+IOL also did not lead to its decrease. After bilateral SLT, compensation of IOP was achieved without local hypotensive therapy (IOP measured by Icare: OD 18.0 mm Hg, OS 15 mm Hg).
<br><b>Conclusion:</b> (I)n order to preserve visual functions, CPE+IOL is highly recommended at the very beginning of PACD, before the formation of GON and goniosynechiae. This is dictated by the dominant role of the lens-involved mechanism in PACD formation, as demonstrated in the described clinical examples.

<b>Purpose:</b> to assess the rate of success of selective laser trabeculoplasty (SLT) in the patients with primary angle closure (PAC) who underwent laser peripheral iridotomy (LPI) but did not achieve intraocular pressure compensation (IOP).
<br><b>Methods:</b> (T)his prospective study included 60 patients with PAC aged 47 to 80 years (30 – with PAC and 30 – with the initial stage of primary angle-closure glaucoma (PACG). All the patients underwent SLT with the trabecular meshwork visualization up to at least 90°. The rate of success was assessed on day 1, at 1 week, 1 month, and 6 months and once a year during 3 years based on the level of IOP, the number of hypotensive drugs used, thickness of retinal nerve fiber layer (RNFL) and ganglion cell complex (GCC), as well as mean light sensitivity (MD). The following predictors of SLT success were studied: corneal hysteresis (CH), corneal resistance factor (CRF), central corneal thickness (CCT), corneal-compensated IOP (IOPcc), anterior chamber depth (ACD), anterior chamber angle (ACA), lens thickness (LT).
<br><b>Results:</b> (I)n both groups, in all periods, there was a significant decrease in IOP (p < 0.05 in all cases) with the maximum decrease on day 1 after SLT, and the minimum after 3 years. At 1 year, there was a significant difference in IOPcc decrease in PAC in comparison with PACG (p = 0.048), which persisted throughout the entire follow-up period (p = 0.008). At 3 years, there were no signs of GON development among the patients with PAC, and the need for hypotensive therapy was significantly lower in PACG at 2 and 3 years of follow-up (p = 0.041 and p = 0.037, respectively). The GON progression rate in PACG was -0.06 ± 0.68 dB/year. The predictors of SLT failure in both groups were determined: low CH, high preoperative IOP and CRF, lower CCT, small ACA and АСD, and increased LT (all p < 0.05).
<br><b>Conclusion:</b> (T)he long-term SLT success is higher in PAC than in PACG, that is associated with a smaller amount of goniosynchia, a deeper anterior chamber, a less increased LT, and therefore, longer duration of laser exposure. SLT is an alternative PAC treatment preventing the development of GON in relation to clear lens extraction.


<b>Purpose:</b> (T)o study the role of the choroid and lens in the development of primary anterior chamber angle closure.
<br><b>Methods:</b> (T)he study included 90 patients aged 47 to 80 years (30 with primary angle closure (PAC), 30 with suspected primary angle closure (PACs), and 30 in the control group) who underwent swept source optical coherence tomography (SS-OCT). The following parameters were analyzed: subfoveolar choroidal thickness (SFCT), intraocular pressure (IOP), axial length (AL), anterior chamber depth (ACD), lens vault (LV), iris curvature (ICurv) and iris thickness (IT750), angle opening distance (AOD500, AOD750), and trabecular-iris space area (TISA500, TISA750).
<br><b>Results:</b> (S)FCT in PAC (341±59 µm) and PACs (340±51 µm) was higher than in the control group (257.0±37.0 µm, p<0.05). In PAC and PACs, the correlations of SFCT with age, AL, LV, ICurv, IT750 were revealed (p<0.05 for each), as well as correlations of LV with age, IOP, ACD, ICurv, IT750, AOD500, AOD750, TISA500, TISA750 were found (p<0.05 for each). The correlation of SFCT with IOP was determined only in PAC (p=-0.476; p=0.008).
<br><b>Conclusion:</b> (T)he increase in the choroidal thickness in macula in both PACs and PAC compared with the controls, as well as the correlations of subfoveolar choroidal thickness with lens vault and iris parameters suggest the involvement of the choroid in the pathogenesis of primary angle closure disease (PACD). The correlations of lens vault with IOP, as well as the parameters of anterior chamber and iris indicate the prevailing role of the lens in the development of PACD and the need for its early replacement.

<b>Purpose:</b>To compare choroidal thickness before and after laser peripheral iridotomy (LPI) and lens extraction (LE) in patients with primary angle closure (PAC).
<br><b>Methods:</b>The prospective study included 60 patients (60 eyes) with PAC aged 41 to 80 years. LPI was performed in 30 eyes, LE was performed in 30 eyes. All patients underwent Swept Source optical coherence tomography. The parameters of the anterior and posterior segments of the eye were analyzed including the choroidal thickness in the macula (in foveola, in diameters of 1 mm, 2 mm and 3 mm from it) as well as intraocular pressure (IOP) and number of medicines.
<br><b>Results:</b>After LE, choroidal thickness significantly increased (from 341±59 to 345±57 μm, p=0.000) in the foveola as well as in all sectors (p<0.05) except for the nasal one, 3 mm from the center of the foveola (p=0.05). After LPI, choroidal thickness significantly increased in all sectors (all p<0.05) except for the superior (p=0.124) and temporal (p=0.103) sectors 3 mm from the center of the foveola as well as in the foveola itself (from 343±58 to 341±60 μm, p=0.519). There was no significant difference in choroidal thickness in the macula between the groups after treatment (all p>0.05).
<br><b>Conclusion:</b>An increase the choroidal thickness in patients with PAC after LPI and LE suggests the involvement of the choroid in the mechanisms of the hypotensive response to the treatment.

Addressing the issue of a closed angle of the anterior chamber plays a key role in preventing the development of angle- closure glaucoma.
<br><b>Purpose:</b> (t)o compare the efficacy of Laser Peripheral Iridotomy (LPI) at the stage of primary angle closure suspects (PACs) with LPI carried out at the initial stage of primary angle-closure glaucoma (PACG).
<br><b>Methods:</b> (A) clinical case of a primary angle closed disease (PACD) in a patient with PACs after LPI in the right eye and with PACG after LPI, selective laser trabeculoplasty (SLT) and phacoemulsification with intraocular lens implantation in the left eye is presented. A detailed examination was performed in dynamics, including methods of visualization of the anterior and posterior segments of the eye.
<br><b>Results:</b> (A)fter 2.5 years, the anterior chamber angle in the right eye retained an expanded profile after LPI (up to 30°), no signs of PACG development were recorded. On the left eye, the anterior chamber angle remained closed (9°) with an IOP of 24 mm Hg at the maximum hypotensive therapy with eye drops. Despite the absence of progression of glaucomatous optic neuropathy in both eyes, the risk of the transition from the initial stage to the moderate and advanced stage of PACG in the left eye still remains due to the presence of goniosynechia and possible fluctuations of intraocular pressure.
<br><b>Conclusion:</b> (L)PI is more effective at the stage of PACs and its implementation is advisable in order to prevent the development of PACG.

<b>Purpose:</b> (t)o compare microcirculatory changes in patients with early stages of primary angle closure disease (PACD) and pri- mary open-angle glaucoma (POAG).
<br><b>Methods:</b> (T)he study retrospectively analyzed the clinical data of 60 eyes with PACD, 30 with initial POAG, and 30 eyes without any ophthalmic pathologies. Vessel density (VD) in the optic nerve head and peripapillary retina (wiVD Disc), as well as in the inner layers of fovea and parafovea (wiVD Macula) and their different sectors were determined in all patients by optical coherence tomography angiography (OCTA). The correlation of VD with axial length (AL), anterior chamber depth (ACD), lens thickness (TL), and corneal-compensated intraocular pressure (IOPcc) was assessed.
<br><b>Results:</b> (T)he wiVD Disc in PACD (42.47±4.23%) was lower than in POAG eyes (47.46±2.10%), p<0.001, but the difference for wiVD Macula was not significant: 41.71±4.55% and 39.29±2.46%, respectively (p=0.47). In both PACD and POAG, all OCTA parameters were lower than in normal eyes: p=0.000 for both wiVD Disc and wiVD Macula. WiVD Disc correlated with ACD both in PACD (r=0.724, p=0.012) and in POAG (r= 0.685, p=0.012), but a correlation with IOPcc was found only in PACD (r= –0.670, p=0.033). The largest number of inverse correlations was found between TL and VD both for wiVD Disc (r= –0.714, p=0.006) and the parameters of macular area (in para- and perifovea).
<br><b>Conclusion:</b> (O)CTA parameters differ significantly from the norm even in the early stages of both PACD and POAG. In PACD, there was a significant decrease in microcirculation in the peripapillary retina compared to POAG, which had an inverse correlation with IOPcc; there was also an inverse correlation of OCTA parameters in the optic nerve head and macula with lens thickness.

<b>The purpose/b> of this work is to review the literature data on the role of optical coherence tomography in the diagnosis of diseases of the closed angle of the anterior chamber. An analysis of the modern technical devices use — optical coherence tomography of the anterior segment (AS-OST) and models with a frequency-modulated source (Swept Source) is presented. The advent of new imaging technologies such as SS-OCT is advancing the understanding of the pathogenesis of primary angle closure diseases. Visualization of the structures of the anterior segment of the eye is an important part of the strategy aimed at solving the problem of identifying risk factors, diagnosing, monitoring and evaluating the effectiveness of treatment of diseases of primary angle closure. Qualitative and quantitative data analysis based on optical coherence tomography significantly increases the diagnostic accuracy, which undoubtedly plays a key role in the choice of treatment tactics for the closed angle of the anterior chamber. The interpretation of research results should take into account the strengths and weaknesses of traditional methods and newly developed technologies.
<br><b>Conclusion:</b> (O)ptical coherence tomography of the eye’s anterior segment is a standard in modern diagnostics and evaluation of the effectiveness of treatment of diseases of primary angle closure, taking into account pathogenetic mechanisms.

Purpose: To evaluate the efficacy of the optimal examination technique for patients with glaucoma during the COVID-19 pandemic that includes one of the safest methods of tonometry [transpalpebral tonometry (TPT), contour dynamic tonometry (CDT) and Icare rebound tonometry (RBT)] in combination with spectral domain optical coherence tomography (SD-OCT) and optical coherence tomography angiography (OCTA). Material and methods: The study included 65 patients with primary open-angle glaucoma (POAG) who sought medical aid at the Ophthalmological Center of FMBA during the COVID-19 pandemic; they were examined using three tonometry methods: RBT, TPT and CDT. All patients underwent central corneal thickness measurement, perimetry, OCT and OCTA with assessment of vessel density (VD) of the superficial plexus in the macula (whole image macula) and peripapillary retina (PPR). Results: High correlation was found between the results obtained with RBT, TPT and CDT. None of the methods showed a correlation between IOP and corneal thickness. The correlations between IOP and OCTA parameters were obtained: IOPTPT and VDPPR in the inferior temporal sector (r= -0.386, p=0.027), IOPRBT and VD whole image macula (r= -0.69, p=0.019), and in the macula inferior hemisphere (r= -0.75, p=0.008), as well as between the ocular pulse amplitude (OPA) and VD in the macular inferior hemisphere (r=0.380, p=0.039). The OCTA parameters had a moderate, but significant correlation with the perimetric indices. Conclusions: Tonometry methods (TPB, CDT and RBT) exhibit high correlation with each other and no correlation with corneal thickness. IOP parameters measured by different methods, especially using the Icare tonometer, correlate with OCTA parameters, and the latter - with perimetric indices. The combination of these tonometry methods with SD-OCT and OCTA is optimal for examining patients during the pandemic.


Outer retinal tubulation (ORT) develops in the later stages of age-related macular degeneration (AMD). It is associated with low visual acuity, severe loss of photoreceptors, choroidal neovascularization (CNV), and geographic atrophy. Despite the frequent detection of ORTs by optical coherence tomography (OCT), their role in the process of outer retinal atrophy and degenerative changes in photoreceptors remains undetermined. Purpose: To investigate the evolution of ORT in patients with exudative and disciform-stage CNV. Material and methods: The retrospective study included 340 patients with AMD, among them 235 (69%) women and 105 (31%) men with mean age of 76±7.4 years; in all, the analysis involved 267 eyes with dry AMD and 174 eyes with CNV: 92 eyes - with exudative AMD, 82 eyes - with disciform-stage disease). In addition to standard OCT, all patients underwent OCT-angiography (OCTA). In 10 cases, patients with exudative AMD were followed up after intravitreal injections of Aflibercept. Results: ORTs were detected in 37 eyes of 32 patients (26%), all of them with CNV: 13 eyes with exudative AMD (group 1) and 24 eyes with disciform scar (group 2; p=0.013). The groups were similar in the type and morphology of ORTs. The most common were closed, i.e. fully formed ORT (92% of cases in group 1, and 88% in group 2). Destruction of the ellipsoid zone associated with ORT was observed in both groups. In one case, there was an increase in the size of ORT corresponding to the volume of cystic macular edema. Disappearance of ORT was noted only in one of ten patients 3 months after intravitreal injection of Aflibercept, but was not accompanied by visual acuity improvement. Conclusion: Outer retinal tubulations are more common in the later stages of AMD, being an indicator of a deep destructive process in photoreceptors. In exudative AMD, ORTs serve as a predictive marker for poor functional outcomes.

The review presents the data on characteristic features of the new coronavirus infection caused by SARS-CoV-2 and the possibility of its transmission through the eye surface and lacrimal fluid, analyzes the information on eye damage caused by COVID-19, and provides the results of a systematic meta-analysis on the subject. The author describes the system for organizing ophthalmological care in the settings of unfavorable epidemiological situation associated with the COVID-19 pandemic, and considers the preventive measures of infection transmission between patients and medical personnel. The article also gives recommendations for sterilizing medical equipment.


Purpose: To compare the role of spectral-domain optical coherence tomography (SD-OCT) in regard to retinal nerve fiber layer (RNFL) and ganglion cell complex (GCC) assessment in the detection of primary angle-closure glaucoma (PACG) and primary open-angle glaucoma (POAG) progression. Materials and methods: In the prospective study, 131 subjects with PACG and POAG were examined during 72 months with follow-up visits every 6 months. Visual field (VF) progression was detected using the Guided Progression Analysis (GPA) of the Humphrey visual field analyzer and structural change using SD-OCT while a significant negative trend for the RNFL and GCC was gauged. The diagnostic accuracy of RNFL and GCC thinning in the detection of glaucoma progression was compared between PACG and POAG eyes using the Kaplan-Meier method with the calculation of the log-rank test. Results: Progression was detected in 57% of eyes with POAG and 59% of eyes with PACG. The rate of thinning of RNFL (-2.95±1.85 μm/y) and GCC (-3.22±2.96 μm/y) was significantly higher in PACG progression eyes compared with POAG [-1.64±2.00 μm/y (P=0.018) and -1.74±2.05 μm/y (P=0.046), respectively]. The progression was associated with initial pattern standard deviation in both glaucoma subtypes, while only in PACG-with long-term intraocular pressure fluctuations (cutoff >5.2 mm Hg) and lens thickness (cutoff >4.92 mm), and only in POAG-with initial focal loss volume of GCC (cutoff >1.5%).In PACG, the rate of the visual function deterioration correlated with GCC thinning rate (r=0.330, P=0.027), but not with the RNFL thinning rate (r=-0.010, P=0.79), while in POAG, it was significant for both RNFL thinning (r=0.296, P=0.039) and GCC thinning (r=0.359, P=0.011). In PACG patients with progressive GCC thinning, functional progression was detected earlier (log-rank test P≤0.001) than in patients with progressive RNFL thinning (log-rank test P=0.457), while for POAG, these results were P=0.012 and ≤0.001 for GCC and RNFL thinning, respectively. Conclusions: SD-OCT plays an important role in detecting PACG progression. In contrast to POAG, GCC thinning predicted functional loss better than RNFL thinning in PACG.

Purpose To study the factors affecting the corneal endothelium after selective laser trabeculoplasty (SLT) in primary open angle glaucoma (POAG) and primary angle closure glaucoma (PACG). Method This prospective interventional study included 56 patients (56 eyes) with POAG and 55 patients (55 eyes) with PACG. All participants received a standard SLT session. Patients with PACG were pretreated with laser peripheral iridotomy for at least 2 months before SLT. Corneal endothelium cell count (ECC), pleomorphism and polymegathism were measured before SLT, as well as at the increments of 1 hour, 1 day, 1 week, 1 month, 3 months and 6 months following SLT using confocal microscopy. A multiple regression analysis was applied to detect the factors affecting the ECC in the long-term post-SLT period. Results In both groups, the mean ECC significantly decreased from the baseline after SLT. While in POAG, corneal endothelium recovered within 1 month, in PACG, its damage persisted throughout the whole follow-up period. According to the multiple analysis, baseline ECC (β=0.891, p=0.000 in POAG and β=0.706, p=0.000 in PACG) and age (β=−0.227, p=0.000 in POAG and β=−0.196, p=0.000 in PACG) were the common risk factors affecting ECC in both glaucoma forms, while the initial anterior chamber depth (β=0.254, p=0.000), only in PACG. The duration of glaucoma treatment (β=−0.317, p=0.043 in POAG and β=−0.302, p=0.047 in PACG) and pigmented deposits on the corneal endothelium in PACG (β=−0.326, p=0.019) were the risk factors determined in the univariate analysis. Conclusion Age and the baseline ECC are the risk factors for corneal endothelium damage after SLT in POAG and PACG. Shallow anterior chamber may affect corneal endothelium in PACG. These data should be considered when choosing an algorithm for glaucoma treatment.

Purpose. To establish the morphological and functional parameters to predict the effectiveness of intravitreal injections (IVI) of ranibizumab in macular edema due to retinal vein occlusion and to develop a mathematical model for personalized treatment algorithms. Material and methods. This is a retrospective study of 98 patients (98 eyes) with macular edema, who received IVI of ranibizumab and were followed up for 12 months. Spectral optical coherence tomography scans and best corrected visual acuity (BCVA) assessments were conducted every 3 months. Treatment outcome predictors were calculated based on logistic regression analysis. Results. The most significant prognostic factors for the long-term BCVA were baseline BCVA (OR 11.1, p = 0.001), foveal volume (OR 10.8, p = 0.001), destruction of external limiting membrane (OR 15.8, p = 0.001), photoreceptor inner/outer segments (OR 11.1, p = 0.001) and retinal pigment epithelium (OR 9.1, p = 0.001). It has also been discovered that post-treatment BCVA correlated with the height of serous retinal detachment (SRD) (r = −0.4, p = 0.001), ganglion cell complex thickness (r = + 0.3, p = 0.01) and focal loss of ganglion cells (r =−0.3, p = 0.005). Patients without SRD required fewer ranibizumab injections (3.8 ± 1.1) for macular edema fluid resorption compared to those with SRD (5.7 ± 1.2, p = 0.03). A mathematical model for predicting and personalized approach therapy of ranibizumab has been obtained (accuracy of 89%). Conclusion. The effectiveness of IVI of ranibizumab depends on baseline morphological and functional changes. The obtained mathematical model allows for predicting the outcomes of therapy, determining individualized algorithms to increase the treatment effectiveness and to prevent low vision that corresponds to the principles of predictive, preventive, and personalized medicine.


Relevance. Choroidal effusion is a complication accompanying both surgical interventions and ophthalmopathies of predominantly inflammatory etiology. The release of proteins from choriocapillaries lumen and decrease of intraocular pressure relative to the pressure in the episcleral veins lead to the choroid detachment. Purpose. To analyze the causal link between choroidal effusion and topical application of carbonic anhydrase inhibitors using a clinical example. Material and methods. The paper describes a clinical case of the development of unilateral recurrent choroidal effusion 13 years after sinus trabeculectomy associated with the use of carbonic anhydrase inhibitors. The first episode of choroidal effusion was induced by a fixed combination of brinzolamide with timolol, while the use of dorzolamide caused the repeated episode. The clinical picture was accompanied by significant decrease in visual acuity related to acute hypotension and severe folds of the descemet’s membrane. Ultrasonic B-scanning revealed the choroid detachment. The dechallenge of carbonic anhydrase inhibitors, the use of anti-inflammatory and cycloplegic drugs contributed to achieve the choroid adherence. Results. This clinical case clearly demonstrates a causal link between choroidal effusion and topical application of carbonic anhydrase inhibitors. The timely drug therapy made it possible to avoid surgical intervention. Intraocular pressure increased later. Brimonidine was prescribed to reduce it, the intraocular pressure was normalized, and the clinical picture stabilized. Conclusion. Ciliochoroidal effusion may occur in the eyes with primary angle-closure glaucoma even several years after surgical treatment in the setting of the use of this group of hypotensive drugs. It is necessary to take a balanced approach to the use of carbonic anhydrase inhibitors in each particular case, including in primary angle-closure glaucoma.

The purpose of this work is to review the literature data on the role of optical coherence tomography in the diagnosis of diseases of the closed angle of the anterior chamber. The analysis of the use of modern technical devices — optical coherence tomography of the posterior segment, models with a frequency-modulated source (Swept Source) is presented. The emergence of new imaging technologies such as SS-OCT contributes to understanding the pathogenesis of primary angle closure diseases in terms of involvement of the choroid in the process. A thicker choroid in the macular area may be an anatomical risk factor for closed angle disease. The expansion of an abnormally thick choroid in combination with the structural features of the anterior segment in eyes with a short axial length, including against the background of psychoemotional stress, can lead to an attack of angle closure. Visualization of the structures of the posterior segment of the eye is an important part of the strategy aimed at solving the problem of identifying risk factors, diagnosing, monitoring and evaluating the effectiveness of treatment of diseases of primary angle closure. Qualitative and quantitative data analysis based on optical coherence tomography significantly increases the diagnostic accuracy, allows to determine its progression and to predict its course. This plays a key role in the choice of treatment tactics for the anterior chamber angle closure. The review considers the effect of local antihypertensive eye drops on the choroid. Conclusion. Optical coherence tomography is a standard in modern diagnostics and evaluation of the effectiveness of treatment of diseases of primary angle closure, allowing a better understanding of the pathogenesis of the disease and its complex nature. Imaging improves the ability to accurately diagnose and choose the right treatment strategy.


Purpose: To study the changes in central corneal thickness (CCT) and corneal hysteresis (CH) after selective laser trabeculoplasty (SLT) in primary open-angle glaucoma (POAG) and primary angle-closure glaucoma (PACG) after laser peripheral iridotomy (LPI) and to determine their effect on the prognosis of the surgery. Material and methods: The prospective study involved 68 eyes with initial PACG after LPI and 74 eyes with initial POAG observed for 6 months. Corneal-compensated IOP (IOPcc), corneal resistance factor (CRF), CH and CCT were studied as the predictors of SLT, which was considered successful when IOPcc decreased by 20% or more from the baseline without additional hypotensive therapy and/or repeated SLT. Results: In both forms of glaucoma, CCT increased within the first hour after SLT: 567±24.08 µm (p=0.001) in POAG, and 572±21.41 µm (p=0.000) - persisting for over a month - in PACG. CCT correlated with laser energy at all stages of the examination both in POAG and PACG patients. The following predictors of SLT failure were determined: CH (p=0.000 in PACG and p=0.001 in POAG), as well as initial IOP (p=0.010 in PACG and p=0.016 in POAG) and CRF (p=0.003 in PACG and p=0.005 in POAG) and CCT (p=0.023 in PACG and p=0.026 in POAG). The value of anterior chamber angle (ACA) was a predictor only for PACG (p=0.011). Conclusion: SLT leads to an increase in CCT, which lasts longer in PACG after LPI than in POAG and correlates with the level of laser energy. Lower CH and initially higher IOP are the common predictors of SLT failure in the long term for both forms of glaucoma. Smaller ACA have a negative prognostic sign in POAG.


Purpose: To assess the progression of primary open-angle glaucoma (POAG) and to study the role of retinal microcirculation in its progression. Material and methods: In this 2-year prospective study, the rate of POAG progression was determined using perimetry (ROP1) and spectral domain optical coherence tomography (SD-OCT) by thinning of retinal nerve fiber layer (RNFL) (ROP2) and ganglion cell complex (GCC) (ROP3). The vessel density of parafoveal superficial plexus (VD parafovea) and peripapillary retina (VD ppr) was assessed using OCT angiography, peripheral resistance index (RI), and blood flow velocity in the posterior short ciliary arteries (PSCA) and central retinal artery (CRA) with the use of color Doppler mapping. The predictive properties of each parameter were calculated using the area under receiver operating curve (AUC). Results: Progression was detected in 9.8% cases by perimetry and in 19.7% cases by OCT. The combination of these two methods increased the detection up to 32.8%. Circulatory parameters - VD parafovea (AUC 0.70±0.07), VD ppr (0.715±0.07), PSCA RI (0.801±0.12), CRA RI (0.798±0.11) - had similar high predictive properties as IOP max (0.79±0.05), corneal hysteresis (0.755±0.07), thickness of inner parafoveal layers (0.728±0.07) and RNFL (0.692±0.06). The study revealed the following correlations: ROP1 with maximum IOP (p=0.01), ROP2 with blood flow velocity in PSCA (p=0.01), VD parafovea with corneal hysteresis (p=0.01), and GCC thickness with ocular perfusion pressure (p=0.01). Conclusion: The obtained data demonstrates the importance of combining perimetry with OCT for detecting the progression of glaucoma and indicates its relationship with reduced ocular hemoperfusion.

Purpose: to compare the factors associated with the progression of primary open-angle glaucoma (POAG) and primary angle closure glaucoma (PACG). Material and methods. This prospective study analyses clinical data of POAG and PACG patients followed up for 6 years. The pro gression of glaucomatous optic neuropathy (GON) was determined using perimetry and spectral optical coherence tomography (OCT). The value of each diagnostic indicator (z-value) was calculated using the Wilcoxon-Mann-Whitney test and the area under the ROC-curve (AUC) to identify the parameters reliably associated with the progression in both groups of patients. Results. According to OCT, 47.3% of PACG patients and 52.46% of POAG patients had GON progressing, while according to perimetry, these figures were 21.8% and 23%, respectively. The common factors associated with progression of these glaucoma forms were age (AUC 0.7, z –1.9 in PACG and AUC 0.7, z –2.9 in POAG) and maximum IOP (0.7; –2.7 in PACG and 0.79; –5.4 in POAG). The progression of PACG is associated with lens size (0.7; –2.4), subfoveal choroidal thickness (AUC 0.8, z –3.3) and peripapillary choroidal thickness (0.79; –3.2), resistive index in the vortex veins (0.81; –3.3) and their end diastolic blood flow velocity (0.83; 3.2). The progression of POAG is associated with a thin peripapillary (0.75; 2.6) and subfoveal choroid (0.74; 2.5), increased resistive index in the posterior short ciliary arteries (0.8; –2.3), and initial retinal nerve fiber layer (RNFL) thickness: 0.69; 2.9. Conclusion. The progression of POAG and PACG has only two common factors — age and maximum IOP. The progression of PACG is mainly related to the lens size, venous dysfunction and the choroid expansion, while the progression of POAG is related to the initial RNFL thickness, reduced arterial blood flow and choroid thinning.

Purpose: To determine the predictors of primary open angle glaucoma (POAG) progression successful monitoring and a personalized treatment approach. This postulate is an integral principle of predictive preventive personalized medicine (PPPM) that is to predict a disease development/progression and targetly prevent it by providing a treatment tailored to the person.


RELEVANCE: The ability of antiglaucoma drugs to improve ocular hemoperfusion is an important aspect of their action. Tafluprost is the first preservative-free prostaglandin analog. The efficacy and safety of tafluprost, as well as tafluprost/timolol fixed combination (FC), were demonstrated in randomized multicenter trials. However, there is no literature on the effect of tafluprost and its FC on the peripapillary and macular blood flow. Purpose: To determine the changes of microcirculation in the optic nerve head (ONH), peripapillary retina, and macula in patients with newly diagnosed primary open-angle glaucoma (POAG) under the topical tafluprost and tafluprost/timolol FC treatment. MATERIALS AND Methods: Optical coherence tomography angiography (OCT-A) was performed in dynamics with an interval of a week in 36 patients (36 eyes) with a newly diagnosed initial stage of POAG: 12 eyes with tafluprost, 12 – tafluprost/timolol FC, and 12 – no topical treatment (the control group). The change in intraocular pressure (IOP), mean ocular perfusion pressure (MOPP) of the eye, and vessel density (VD) inside the ONH (inside disc), as well as in the peripapillary retina and macula, was evaluated by comparing paired repeated observations using the median growth analysis. Results: In the tafluprost group, there were a decrease in IOP by 19.4% and an increase in MOPP by 8.7% from the reference level. In the tafluprost/timolol group, these figures were 43% and 30.1%, respectively. OCT-A values did not change reliably, except for VD inside disc: the median growth of the tafluprost group was 2.28 (P = 0.02) and of the tafluprost/timolol group was 1.82 (P = 0.03). These changes were obtained in 11 of 12 patients in each group under treatment. In control group, all indicators remained unchanged. ConclusionS: A significant increase of MOPP and a decrease of VD in the ONH in patients with initial glaucoma occurred within a week under the topical tafluprost or its FC. This can be explained by the restoration of autoregulation of the ocular blood flow in conditions of pronounced hypotensive effect of the drugs.


Purpose: To compare the ability of SLT in preventing glaucoma progression in the initial primary angle-closure glaucoma (PACG) after laser peripheral iridotomy and primary open-angle glaucoma (POAG) in the long term. Methods: 60 patients with the initial stage of PACG after laser peripheral iridotomy and 64 initial POAG patients were recruited in a prospective study. Complete success of selective laser trabeculoplasty (SLT) was defined as a 20% intraocular pressure (IOP) reduction with topical hypotensive medications without any hypotensive intervention. Pre-SLT rate of progression and post-SLT rate of progression (ROP) was detected in the both groups by means of the trend and the event analysis of perimetry, the Guided Progression Analysis, and the optical coherence tomography- (OCT-) based negative trend for either the thickness of the peripapillary retinal nerve fiber layer (RNFL) or ganglion cell complex (GCC). Results: IOP decreased significantly after SLT in both the groups. 30% in PACG and 19% in POAG had the progression according to perimetry and 49% in PACG and 40% in POAG had the progression, respectively, according to OCT. After SLT, ROP was reduced from -0.14 ± 0.39 dB/year to -0.08 ± 0.48 dB/year, p=0.034, in PACG and from -0.09 ± 0.36 dB/year to -0.04 ± 0.43 dB/year, p=0.021, in POAG. According to RNFL trend analysis, ROP was reduced from -1.86 ± 2.9 μm/year to -1.38 ± 2.2 μm/year, p=0.039, and from -1.24 ± 2.23 μm/year to -0.76 ± 1.73 μm/year, p=0.037, in PACG and POAG, and according to GCC, ROP was reduced from -1.88 ± 2.9 μm/year to -1.34 ± 2.0 μm/year, p=0.040, and from -1.35 ± 2.16 μm/year to -0.91 ± 1.86 μm/year, p=0.040, in PACG and POAG, respectively. ROP was significantly faster in PACD than in POAG between 2 and 6 years after SLT: -0.15 ± 0.46 dB/year and 0.02 ± 0.38 dB/year (p=0.042). However, it did not differ significantly according to OCT. Conclusion: SLT is an effective treatment for initial PACG after LPI and POAG that can prevent functional and structural deterioration in the long term.

Relevance: Vascular factors may be involved in the development of both high tension glaucoma (HTG) and normal tension (NTG) glaucoma; however, they may be not exactly the same. Autonomic dysfunction characterized by heart rate variability (HRV) is one of the possible reasons of decrease in mean ocular perfusion pressure (MOPP). Purpose: To compare the shift of the HRV parameters in NTG and HTG patients after a cold provocation test (CPT). Methods: MOPP, 24-hour blood pressure and HRV were studied in 30 NTG, 30 HTG patients, and 28 healthy subjects. The cardiovascular fitness assessment was made before and after the CPT. The direction and magnitude of the average group shifts of the HRV parameters after CPT were assessed using the method of comparing regression lines in order to reveal the difference between the groups. Results: MOPP and minimum daily diastolic blood pressure were decreased in HTG and NTG patients compared to healthy subjects. There was no difference in MOPP between HTG and NTG before the CPT. However, all HRV parameters reflected the predominance of sympathetic innervation in glaucoma patients compared to healthy subjects (P < 0.05).Before the CPT, the standard deviation of NN intervals (SDNN) of HRV was lower in HTG compared to NTG, 27.2 ± 4.1 ms and 35.33 ± 2.43 ms (P = 0.02), respectively. After the CPT, SDNN decreased in NTG by 1.7 ms and increased in HTG and healthy subjects by 5.0 ms and 7.09 ms, respectively (P < 0.05). The analysis of relative shift of other HRV parameters after the CPT also revealed a significant difference between NTG and HTG in regard to the predominance of sympathetic innervation in NTG compared to HTG. Conclusion: Patients with NTG have more pronounced disturbance of autonomic nervous system than HTG patients, which is manifested with the activation of sympathetic nervous system in response to CPT. This finding refers to the NTG pathogenesis and suggests the use of HRV assessment in glaucoma diagnosis and monitoring.


Purpose: To evaluate the efficacy of selective laser trabeculoplasty (SLT) for patients with primary angle-closure glaucoma (PACG) following a YAG laser peripheral iridotomy (PI) in comparison with primary open-angle glaucoma (POAG) and to assess the predictors of outcome of SLT. Patients and methods: In retrospective study 68 patients with PACG after PI (68 eyes) and 74 POAG patients (74 eyes) were observed for 6 years. The effectiveness of SLT (20% reduction of intraocular pressure) was assessed using Kaplan-Meier survival analysis. The parameters for distinguishing the eyes with success and failure of SLT were detected by means of area under receiver operating characteristic curve (AUC). The predictive factors affecting SLT outcome were determined using Cox-regression analysis. Results: The success ratio was 87% in both groups in 1 year and dropped to 4% in PACG and to 6% in POAG in 6 years. Corneal hysteresis [odds ratio (ОR)=0.367, Р=0.005 for PACG, ОR=0.446, Р=0.008 for POAG] and age (OR=1.182, P=0.012 for PACG, OR=1.164, P=0.002 for POAG) were detected as the predictors of SLT outcome. In PACG pre-SLT anterior chamber depth was additional predictor (ОR=0.242, Р=0.001). The number of pre-SLT pressure-lowing medications was higher in the eyes with SLT failure (AUC, 0.794; P=0.0005 in PACG and AUC, 0.760; P=0.014 in POAG). Conclusions: One-year efficacy of SLT in POAG and PACG after PI was high, but it was reduced in long-term period. Corneal hysteresis, age, and number of pre-SLT hypotensive eye drops were significant prognostic factors for treatment success in both glaucoma forms. In PACG pre-SLT anterior chamber depth affected the SLT outcome.


Purpose: To compare the diagnostic accuracy of structural parameters, vessel density (VD) measured by optical coherence tomography angiography (OCTA), and electrophysiological testing in diagnosis of primary open-angle glaucoma (POAG). Methods: 35 healthy participants and 90 POAG subjects underwent the measurement of whole image en face (wi) VD in the disc/peripapillary region and macula, the retinal nerve fiber layer (RNFL), and the average thickness of ganglion cell complex (GCC), pattern electroretinograms and pattern visual evoked potentials. The area under the receiver operating characteristic curve (AUC) was assessed for each parameter to differentiate early POAG from healthy eyes and between the POAG stages. Results: To distinguish early POAG from healthy eyes, the parameters with the highest AUC were detected: P50 amplitude of transient pattern electroretinogram, 1° (AUC 0.93, p = 0.002), P1 component of steady-state pattern electroretinogram (AUC 0.92, p = 0.003), P100 amplitude of pattern visual evoked potential, 1° (AUC 0.84, p = 0.013), wiVD macula superficial (AUC 0.80, p = 0.001), wiVD Disc (AUC 0.74, p = 0.016), GCC (AUC 0.74, p = 0.016) and to distinguish early POAG from the moderate to severe POAG: inferotemporal peripapillary VD (AUC 0.94, p < 0.0001) and focal loss volume of GCC (AUC 0.92, p < 0, 001). Conclusions: Our results demonstrate the importance of measuring the microcirculation parameters in the macular area along with PERGs and PVEPs for the early detection of glaucoma. VD in the inferotemporal sector of the peripapillary retina and focal loss volume of the GCC are important for monitoring of the disease. The inclusion of OCTA, PERGs and PVEPs in glaucoma diagnostics may improve its early detection and monitoring.


Primary vascular dysregulation (PVD) is believed to be a main cause of local vasospasm and impaired autoregulation as a possible contributing factor in the pathogenesis of normal tension glaucoma (NTG). Subjects with PVD respond stronger to psychological stress. Autonomic dysfunction is another reason of instable ocular blood flow and may be studied by means of assessment of heart rate variability (HRV) especially during a hand-cold provocation test (CPT).To compare the shift of HRV parameters in NTG and healthy subjects after a cold provocation test and to assess the relation between structural damage, circulatory parameters and autonomic dysfunction in NTG.HRV was studied using CPT in 78 NTG patients and 60 health control matches. The ocular blood flow was measured using color Doppler imaging (CDI). The 24 hours blood pressure (BP) monitoring was carried out. The cardiovascular fitness assessment was made to all patients before and after CPT. Mean group difference of HRV parameters was compared between NTG and healthy subjects using the Euclidean metric. The mean ocular perfusion pressure (MOPP) was measured. Optic nerve head and retinal nerve fiber layer (RNFL) were evaluated using spectral-domain optic coherence tomography (SD-OCT). The relation between HRV, CDI, and SD-OCT-parameters was assessed.In contrast to healthy subjects, a predominance of the sympathetic activity after the CPT was revealed in the NTG group. The end diastolic velocity (EDV) in central retinal artery (CRA) and short posterior ciliary artery (SPCA) was significantly reduced in NTG compared to healthy eyes. In NTG, the main HRV parameter characterizing the total effect of autonomic blood circulation regulation (SDNN) correlated with MOPP (0.75, P = .035), SPCA EDV (0.93, P < .001), and CRA EDV (0.9, P < .001). The average daily diastolic BP correlated with RNFL (0.67, P = .009).The NTG patients have the disturbance of the autonomic nervous system, which increases in response to stress provocation and is related to ocular blood flow and structural damage.

Purpose: To examine the relationship between the development of bioelectric response of retinal cell elements to pattern stimulus and the ocular blood flow. Material and methods: Electrophysiological studies, including pattern-reversal visual evoked potentials (VEP) with large 1 degree (1°) and small 0.25° checks, Color Doppler imaging (CDI) of the retrobulbar vessels, and OCT Angiography in the area of the optic disc and peripapillary retina were performed in 48 patients with initial primary open-angle glaucoma (POAG), 47 patients with advanced POAG, and 42 control subjects. Authors also studied the correlations between VEP values and the parameters used in CDI and OCT-A examination. Results: The most noticeable differences between the study groups were the amplitudes of P100 pattern VEP values for small and large patterns and the OCT-A parameters: Whole-image Disc Vessel Density (widVD), Peripapillary Vessel Density (pVD), Peripapillary Vessel Density Inferior Temporalis (pVD IT). In initial glaucoma, a strong correlation was observed between the amplitude of P100 pattern VEP 1° and pVD IT (r=0.75; p<0.0001); the blood flow rates in ophthalmic artery, central retinal artery, central retinal vein and short posterior ciliary arteries were below normal, while the blood flow in these vessels had statistically reliable correlation with the amplitude of P100 pattern VEP (p<0.05). No correlation was found in patients with advanced stages of glaucoma. Conclusion: Pattern VEP is an informative method of glaucoma diagnostics which accuracy can be enhanced by combining it with OCT-A blood flow examination.

Pattern electroretinogram and macular perfusion in glaucoma Purpose: To study microcirculatory and functional changes in macula in patients with Primary Open-Angle Glaucoma (POAG). Material and methods: The study included 95 POAG patients and 42 healthy control subjects. Whole en face image vessel density (wiVDRetina) was measured both in fovea and in parafovea using OCT-angiography (OCT-A) by means of SD-OCT AngioVue on Avanti RtVue xR (Optovue Inc., U.S.A.). Macular thickness and parameters of macular ganglion cell complex (GCC) were measured on the same day. Blood flow in the retrobulbar vessels was evaluated by means of Color Doppler Imaging (CDI). Pattern electroretinogram (PERG) was also taken from the study eyes. Correlations between PERG, SD-OCT GCC, macular thickness, and the parameters of OCT-A and CDI were studied. Results: The amplitude of t-PERG P50 decreased from 6.1±1.3 µV in normal eyes to 2.8±1.6 µV (p<0.0001) in early glaucoma and to 2.3±1.5 µV (p=0.93) in advanced stages. Relative vessel density of the capillary bed decreased from 51.3±3.0% in normal eyes to 45.9±5.0% (p<0.001) and to 41.8±5.0% (p=0.023) in early and advanced glaucoma respectively. The parameters of OCT-A and CDI correlated with morphological and functional parameters in normal and early glaucomatous eyes. Conclusion: The study revealed reduction of macular microcirculation and decrease of PERG in early glaucoma. Correlations between the circulatory parameters and functional changes were found in early stages of the disease.


Purpose: To compare the diagnostic value of ocular blood flow parameters and choroidal thickness (CT) with standard structural parameters for early glaucoma detection. Methods: A total of 32 patients with pre-perimetric glaucoma were compared with 30 age-matched normal subjects. The thickness of the ganglion cell complex (GCC), retinal nerve fiber layer (RNFL), and the choroid and foveal loss volume (FLV) were measured by means of optical coherence tomography (OCT). Retrobulbar blood velocities (Color Doppler Imaging), corneal compensated intraocular pressure (IOPcc), and corneal hysteresis (CH) were also evaluated. Mean ocular perfusion pressure (MOPP) was calculated by measuring IOP and mean arterial blood pressure as MOPP = ([2/3 diastolic BP + 1/3 systolic BP] × 2/3-IOP). The value of each diagnostic indicator (z-value) was calculated using the Wilcoxon-Mann-Whitney test and the area under the receiver operating characteristic curve (AUC). Results: The following indicators had the largest AUC and diagnostic value (z-value): mean blood flow velocity in the vortex veins (AUC 1.0; z-value 5.35) and central retinal vein (0.85; 3.74), diastolic blood flow velocity in the central retinal artery (0.73; 2.74) and lateral short posterior ciliary arteries (0.71; 2.53), IOPcc (0.74; -2.9), CH (0.69; 2.24), CT (0.69; -2.28), GCC (0.67; 2.05), and FLV (0.66; -1.86) to discriminate pre-perimetric glaucoma from healthy subjects. Conclusions: Interestingly, ocular hemodynamic parameters performed better than structural parameters in detecting early glaucoma. This highlights the potential of techniques to measure ocular blood flow in glaucoma diagnostics independently of the question whether perfusion abnormalities are a cause or a consequence of the disease.

Aim: to assess macular blood flow in primary open-angle glaucoma (POAG) patients using optical coherence tomography angiography (OCT-A). Material and methods: The study included 65 POAG patients and 22 age-matched healthy volunteers. Using OCT-A, blood flow parameters (Flow Area, Flow Index, and Vessel Density) were assessed in the para- and perifovea (0.6-2.5 mm and 2.5-5.5 mm, respectively) at the level of both superficial and deep vascular pexuses. Statistical analysis was performed with SPSS version 21 and MASS library of the R language. Results: All the studied parameters were decreased in glaucoma patients as compared to healthy participants: Index superficial parafovea was 0.03±0.01 and 0.04±0.01 (p<0.001), respectively; Index superficial perifovea - 0.02±0.01 and 0.04±0.01 (p<0.001), respectively; Flow superficial parafovea area - 1.57±0.85 mm2 and 2.53±0.53 mm2 (p<0.001), respectively; Index deep parafovea - 0.02±0.02 and 0.03±0.01 (p<0.001), respectively; Index deep perifovea - 0.01 ±0.01 and 0,03±0.01 (p<0.001), respectively; and Flow deep parafovea area 1.02±0.9 mm2 and 1.97±0.82 mm2 (p<0.001), respectively. The differences were statistically significant between glaucoma patients and the controls, but not between glaucoma patients at different disease stages. Conclusion: Decreased OCT-A parameters in non-advanced glaucoma indicate an early reduction of blood supply to the macula and explain the involvement of the latter in the pathological process in POAG.

Purpose: To assess vascularity of the macular area in patients with glaucoma using optical coherence tomography angiography (OCT-A) and evaluate the role of its examination in early glaucoma diagnosis. Materials and Methods: Thirty-eight eyes of patients with the early stage of primary open-angle glaucoma (POAG), 27 eyes of patients with the advanced and far-advanced stages of POAG, and 22 eyes of age-matched healthy subjects were examined using spectral-domain OCT-A (SD-OCT-А) (RtVue xR Avanti with the AngioVue software, San Jose, CA, USA) in order to measure retinal thickness and angio flow density (AFD) retina in macula (an area bounded by a circle with a diameter of 3 mm), inсluding fovea and parafovea regions (superficial and deep) of the inner retinal layers. The AFD disc and peripapillary flow density were measured in optic nerve head (ONH) and 750-μm-wide elliptical annulus extending from the optic disc boundary. Retrobulbar blood flow parameters, including ophthalmic artery (OA), central retinal artery (CRA), short posterior ciliary arteries (PCAs), central retinal vein (CRV), and vortex veins (VV), were measured by color doppler imaging (CDI). The average thickness of the ganglion cell complex (avg GCC), retinal nerve fiber layer (RNFL), and choroid, as well as the focal loss volume (FLV) and global loss volume (GLV) of GCC were measured by means of SD-OCT. Automated perimetry was performed using Humphrey perimeter (Carl Zeiss Meditec, Dublin, CA, USA). Corneal-compensated intraocular pressure (IOPcc) and corneal hysteresis (CH) were determined using ocular response analyzer. Mean ocular perfusion pressure (MOPP) was calculated by measuring IOP and arterial blood pressure (BP) immediately prior to OCT and using formula: MOPP = (2/3 diastolic BP + 1/3 systolic BP) × 2/3 – IOP. Statistical analysis was performed using SPSS version 21 and MASS library in the R language. As a measure of the parameter’s importance in distinguishing patient groups, a value of the adjusted standardized statistic of the Mann-Whitney test (z-value) and an area under the receiver operating characteristic (ROC) curve (AUC) were used. Results: Although all structural parameters and indices of retrobulbar blood flow were reduced in early glaucoma as compared to the normal controls, the following parameters were the main discrepancy criteria when discriminating these patient groups: macular vascular density-AFD Retina Superficial Whole En Face (z=3.86, p<0.0001; AUC 0.8 (0.69-0.90) and macular thickness in the inferior sector ILM-RPE (z=3.86, p<0.0001; AUC 0.8 (0.69-0.91)). In discriminating early glaucoma from the advanced and far advanced stages of the disease, the most useful were: AFD Disc Peripapillary Inferior Temporalis (z=5.61, p<0.0001; AUC 0.94 (0.86-1.0)) and mean flow velocity in CRA (z=4.16, p<0.0001; AUC 0.81 (0.69-0.92)). Conclusions: The present study revealed the significance of OCT-A for the early diagnosis of glaucoma and the priority of the investigation of the macular microcirculation and its thickness in the inferior sector. These results allow understanding the cause of the early involvement of the macular inner layers in the pathological process in glaucoma.

Purpose: To study venous blood flow of the eye and the correlation between clinical data and ocular blood flow in primary open angle glaucoma (POAG). Methods: Color Doppler imaging of arterial and venous blood flow was performed in 78 patients with normal tension glaucoma (NTG), 80 patients with high pressure glaucoma (HPG) and 60 control subjects. The statistical analysis included the calculation of correlation between clinical data and ocular blood flow parameters as well as Pearson’s correlation coefficient. The threshold P value for statistical significance was 0.05. Results: Ocular blood flow (both arterial and venous) was significantly reduced in NTG and HTG in comparison to the control group. While arterial blood flow reduction was more significant in HTG than in NTG, venous blood flow decrease was more marked in NTG. In contrast to the control group, POAG patients showed a correlation between clinical data and venous blood flow. The correlation was higher in NTG patients. Conclusions: The obtained results indicate the potential importance of venous blood flow in glaucoma pathogenesis,especially in NTG

The new term Flammer syndrome describes a phenotype characterized by the presence of primary vascular dysregulation together with a cluster of symptoms and signs that may occur in healthy people as well as people with disease. Typically, the blood vessels of the subjects with Flammer syndrome react differently to a number of stimuli, such as cold and physical or emotional stress. Nearly all organs, particularly the eye, can be involved. Although the syndrome has some advantages, such as protection against the development of atherosclerosis, Flammer syndrome also contributes to certain diseases, such as normal tension glaucoma. The syndrome occurs more often in women than in men, in slender people than in obese subjects, in people with indoor rather than outdoor jobs, and in academics than in blue collar workers. Affected subjects tend to have cold extremities, low blood pressure, prolonged sleep onset time, shifted circadian rhythm, reduced feeling of thirst, altered drug sensitivity, and increased general sensitivity, including pain sensitivity. The plasma level of endothelin-1 is slightly increased, and the gene expression in lymphocytes is changed. In the eye, the retinal vessels are stiffer and their spatial variability larger; the autoregulation of ocular blood flow is decreased. Glaucoma patients with Flammer syndrome have an increased frequency of the following: optic disc hemorrhages, activated retinal astrocytes, elevated retinal venous pressure, optic nerve compartmentalization, fluctuating diffuse visual field defects, and elevated oxidative stress. Further research should lead to a more concise definition, a precise diagnosis, and tools for recognizing people at risk. This may ultimately lead to more efficient and more personalized treatment.


A complex of neuroprotective therapy, including a new Russian neuropeptide semax, was used in the treatment of glaucoma patients with normalized ophthalmic tone. Electrophysiological and computer methods of examination demonstrated the advantages of new therapy over traditional neuroprotective treatment for glaucoma. The efficiency is due to pathogenetic activity of semax possessing both neuroprotective and neurotrophic effects.

The content of nitrite (final metabolite of nitroradical) was measured in aqueous humor of patients with glaucoma and cataract. The level of NO formation is increased at the initial stage of glaucoma and decreases with the disease progress. A direct correlation between the level of nitrite in aqueous humor and coefficient of easiness of its discharge was detected. Cataract is associated with a high level of nitrite in intraocular fluid. The results are discussed from the viewpoint of ocular hydro--and hemodynamic regulation and NO involvement in the free radical oxidation reactions, playing an important role in the pathogenesis of both diseases.

Lenses from patients with glaucoma and senile cataract (control) were examined under electron microscope. Ultrastructural changes in the lenses of glaucoma patients differ from changes in senile cataract by a more pronounced thinning of the capsule and development of microdefects in it and in many cases by accumulation of amorphous material on the surface of the posterior capsule adjacent to the vitreous body. This material may be pseudo-exfoliate or a manifestation of stratification of the posterior capsule proper. Development of a pseudomembrane on the surface of posterior capsule is a manifestation of proliferative processes in glaucoma. These features in a certain measure reflect the mechanism of cataract development in glaucoma, which helps plan the measures for preventing it. The status of posterior lenticular capsule in glaucoma is to be taken into consideration when implanting intraocular lenses.

